The Modern Decline of Grains
The paleolithic period has found its way into modern history with the abolishment, or at least a dramatic decrease in grain and dairy consumption. The amount of grains we consumed during the paleolithic period is debatable since there is evidence of grain consumption during this time. However, our genes, folic acid fortification, rising blood sugar levels, gluten sensitivity and the current environment make a case for the exclusion of many grains, if any at all.
The Double-Edged Sword of Folic Acid in Grain Products and Supplements
First, you should know that folic acid is different than folate. Folic acid is a synthetic form that is chemically different than the folate found in food. A significant proportion of the U.S. population has low folate levels. Folate deficiency causes massive incorporation of uracil into human DNA (4 million per cell) and chromosome breaks leading to cancer and cognitive defects.
Grain fortification with synthetic b-vitamins like folic acid was implemented to prevent neural tube defects, however, fortification with synthetic folic acid has brought some serious concerns for a certain percentage of the population.
In a study titled Is Folic Acid Good for Everyone? the author argues that folic acid could interfere with the metabolism, cellular transport, and regulatory functions of the natural folates that occur in the body by competing with the reduced forms for binding with enzymes, carrier proteins, and binding proteins. The folate receptor has a higher affinity for folic acid than for methyl-THF—the main form of folate that occurs in the blood and might inhibit the transport of methyl-THF into the brain.
Folic acid is first reduced to dihydrofolate and then to tetrahydrofolate before it can enter the folate cycle. Dihydrofolate reductase (DHFR), catalyzes both these reactions but has been little studied in humans. Enzyme activity varies markedly between individuals with genetic mutations, and therefore it is possible that plasma concentration of unmetabolized folic acid will vary between individuals according to their DHFR activity. High folic acid will also cause dihydrofolate to inhibit MTHFR.
One could postulate that those with a slow DHFR could be more prone to the potential detrimental qualities of high folic acid including cognitive decline when combined with low B12, found mainly in vegetarians and the elderly. In terms of cancer and folic acid, folate has a dual effect on cancer, preventing it but also progressing it once cancer has established.
A 2006 study found that food folate intake was not significantly related to breast cancer risk, but total folate intake, mainly from folic acid supplementation, significantly increased breast cancer risk by 32%.
Another 2006 study found that unmetabolized folic acid was associated with reduced natural killer cell cytotoxicity in postmenopausal women.
A 2012 meta-analysis found that cancer incidences were higher in the folic acid-supplemented groups than the non-folic acid-supplemented groups.
A 2013 meta-analysis, however, did not find any significant effect on cancer incidence.
What we need to explore is the enzymatic activity of the individual’s DHFR, MTHFR and possibly other gene mutations in the methylation cycle when examining the potential negative effects of circulating and unmetabolized folic acid, and at what level certain people need to be more cognizant of avoiding fortified foods and folic acid supplementation.
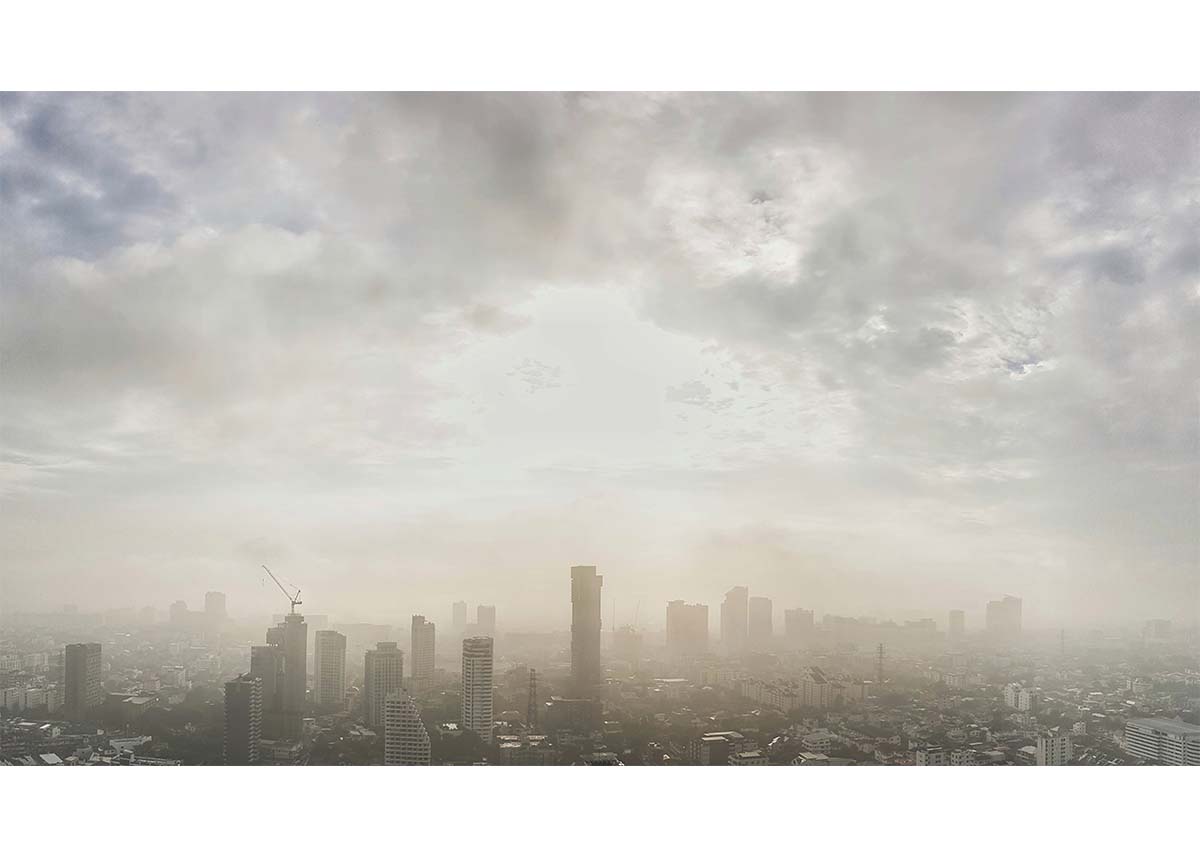
The Environment Has Changed, and So Should Our Grain Consumption
You may have heard of Polycystic Aromatic Hydrocarbons (PAH). Carcinogenic concerns are brought up due to the consumption of smoked and barbecued foods over an open flame where these are created. This concept has always perplexed me because for a million years we have cooked over an open flame. And if you look at the cytochrome P-450 enzymes, you will see we are designed to deal with PAH’s. If you have certain gene variants in these enzymes like CYP1B1 or CYP1A2, your ability to detox these is much lower.
PAH’s in a Vegetarian Diet vs. an Omnivore Diet
After digging a little bit more, it becomes clear that it isn’t meat and smoked food that is the primary problem; it is our environment and the plants that are trapping these compounds in elevated amounts. It is grains, vegetables grown by freeways and vegetable oils that are trapping the most PAH’s, and therefore our consumption of these grains, vegetable oils, and grain-fed animals becomes seriously problematic (also true for aflatoxin B1 with dairy, especially with climate change).
In an analysis of PAHs in the UK diet, it was found that the major contributions came from grains (about one-third) and from vegetable oils and fats (also one-third) with fruits, vegetables and sugars contributed to the remainder. The amount from meat, fish, milk, and beverages was comparatively minor, however, they would be higher in other climates and cultures.
Therefore it could be said that a vegetarian diet high in vegetable oils and grains may contain more PAH’s than a diet with moderate smoked and barbecued meat and fish consumption. A combination of high amounts of grains, vegetable oils, and barbecued meat would be the worst (every fast food restaurant).
Since a large proportion of cancers are attributable to dietary factors, we have to factor in environmental toxins into our food chain. Human exposure to carcinogenic PAH’s is therefore predominately from grains and vegetable oils, not moderate amounts of barbecued meat and smoked fish. If you have gene variants in your detox enzymes, you need to be more conscious about keeping PAH’s low in your diet and following the strategies in the Nutrition Genome Report to lower the carcinogenic effect.
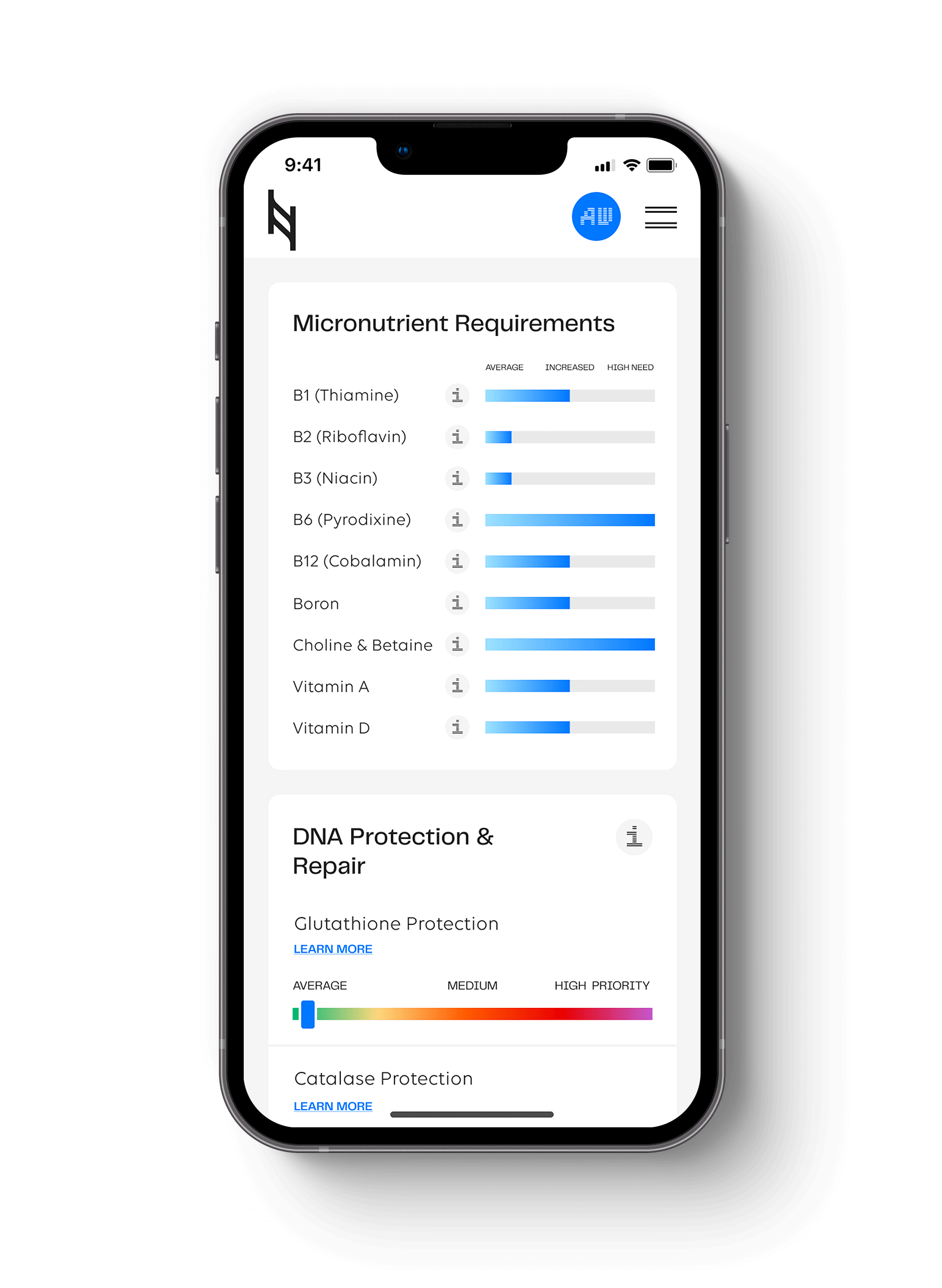
Hit your health goals faster
We'll help you remove the guesswork
Experience the most advanced nutrigenomic test available, covering 100 clinically relevant genes for a "whole body" analysis. Take control of your health today.
$359