It is important to note that the latest research has pointed out that hypertension is more common in the elderly where it has been found to increase the risk of COVID-19 severity by 2.5 times, but the correlation does not necessarily imply that high blood pressure carries the same risk for every age group.
Blood pressure goes up with age and the risk changes with ancestry. Approximately 26% of the world population has high blood pressure, and African Americans have a 45% higher risk of hypertension than all other ethnicities.
Genes: Genes may influence approximately 30% of blood pressure variation in the population. The number of genes implicated in hypertension is quite vast. We will only explore a few of the major ones in this article.
Report Section: Cardiovascular Health and Exercise Performance (AGTR1 and ADD1)
Clinically Significant Genotype: AGTR1 (CC) and ADD1 (TT in Asians)
Ancestral Backstory
Age-related increases in blood pressure have been observed in almost every population, except among hunter-gatherers and farmers. High physical activity, low-stress levels, and potentially protective diets high in fruits, vegetables, potassium, lower in calories, salt, and alcohol are the major contributing factors to the stark differences.
Closer proximity to the equator, higher temperatures, ultraviolet radiation, summertime, and longer hours of sunlight have been associated with lower blood pressure. Distances further from the equator with fewer hours of sunlight and winter has been associated with higher blood pressure levels. Yet, Latin-Americans have a prevalence of high blood pressure 40% higher than that of controls in the rest of the world while the UK has the lowest rate of high blood pressure in Europe.
Countries closer to the equator can grow a higher variety of fruits and vegetables throughout the year compared to Northern Europe, yet, many of these countries have increased sugar and fat in place of fruits and vegetables, and decreased physical activity. Their genetics may be hard-wired for a much higher plant intake and physical activity for healthy blood pressure levels.
In 2015, a study in The Lancet found that central and eastern Europe, sub-Saharan Africa, and South Asia had the highest blood pressure levels. In Canada, Australia, and parts of Europe, blood pressure dropped from 1975 to 2015, with a major contributing factor being diet. Researchers also found that high blood pressure has a stark difference based on socioeconomic levels, with wealthier countries having lower blood pressure and developing countries having higher blood pressure on average.
All of this tells us that the epigenetic impact of diet, lifestyle, and the environment is much more influential than a genetic predisposition to high blood pressure. Our genetics reveal what aspect of the diet and environment we are going to be the most sensitive to changing from our ancestors in regards to blood pressure and how we can target those sensitivities.
Immunity
The AGTR1 A1166C is a new gene addition to the Nutrition Genome Report. Polymorphisms affect the receptor expression and activity of AGTR1, with the CC genotype being the most associated with AGTR1 up-regulation in gene activity. This up-regulation was shown in research to predict the development of hypertension, cardiovascular disease, metabolic syndrome and non-alcoholic fatty liver disease (NAFLD) from excess fat and sugar/carbohydrates in the diet, with fat being the major modifier.
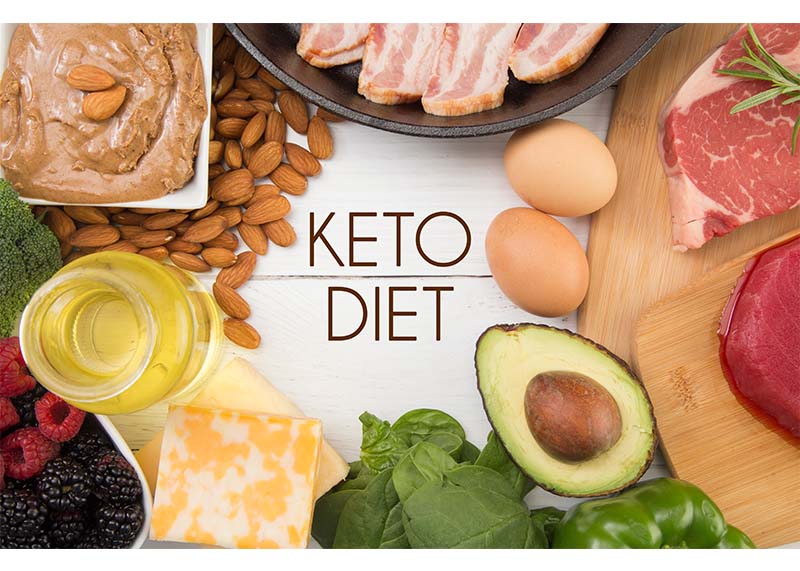
The NF-kb pathway is a downstream target of AGTR1. NF-kb is activated by viruses, which causes an inflammatory response. If left unchecked, this can cause viruses to replicate and become more aggressive. For those with variants in AGTR1, a high-fat intake combined with excess sugar and carbohydrates can activate NF-kb, putting the body in an inflammatory state and making it easier for viruses to become aggressive.
The type and amount of dietary fat changes and increases as you get further from the equator and with the season, while plant life goes down. Carbohydrate intake has been found to be higher the closer you get to the equator, and lower the further you go north of the equator. Therefore, combining a high-fat diet along with a high carbohydrate intake upsets the macro balance, and is especially problematic for the CC genotype of AGTR1.
ADD1 is an existing gene in the Nutrition Genome Report that has a higher incidence of correlation with Asian populations. A meta-analysis of 33 studies with 40,432 participants found that variants in ADD1 rs4961 were significantly associated with hypertension in Asians. Other research has found that salt reduction and an increase in potassium lowers blood pressure by 10 mmHg points compared to rs4961 GG genotypes similarly treated.
Action Plan
- Check your blood pressure. Approximately 1 in 5 people in the US have hypertension and do not know it.
- Check your omega-3 requirements with the FADS2 gene in the Digestion section of the Nutrition Genome Report. A meta-analysis found that omega-3 fatty acids were more effective than increasing physical activity and restricting alcohol and sodium to lower blood pressure.
- If you are male and have high blood pressure, get your testosterone checked. Men whose testosterone levels were slightly above average were 45% less likely to have high blood pressure. Vitamin A, vitamin D, magnesium, zinc, and compound weight lifting exercise (like squats) increase testosterone and help lower blood pressure.
- If you are post-menopausal and have high blood pressure, increase your phytoestrogen intake. Phytoestrogens have been found to lower blood pressure in post-menopausal women in multiple studies. In a Mediterranean study, specific phytoestrogens found in hummus, peanuts, miso soup, tahini sauce, and cruciferous vegetables (broccoli, cabbage, kale, Brussels sprouts) were the most effective.
- If you have high blood pressure and the AGTR1 homozygous genotype, check your folate requirements with MTHFR, and your vitamin C requirements with SLC23A1 to see if nitric oxide levels need improving. Nitric oxide down-regulates AGTR1, balancing out the variant up-regulation and blood pressure. Other precursors to healthy nitric oxide levels include L-arginine, magnesium, vitamin D, DHA, and leafy green vegetables.
- If you have high blood pressure and live in an area of higher pollution, check your SOD2 and GPX1 gene to see if inflammation is a significant reason for high blood pressure, and more antioxidant intake is needed.
- Psychological or emotional stress can contribute to high blood pressure, and deep breathing or meditation practices can help lower it. A meta-analysis evaluated nine randomized, controlled trials using transcendental meditation as a primary intervention for hypertensive patients. The method of transcendental meditation was associated with approximate reductions of 4.7 mm systolic blood pressure and 3.2 mm diastolic blood pressure.
Sources
1. https://academic.oup.com/aje/article/183/11/1071/2739312
2. https://www.cdc.gov/bloodpressure/facts.htm
3. https://www.heart.org/en/coronavirus/coronavirus-covid-19-resources/keeping-a-lid-on-blood-pressure-during-the-coronavirus-crisis
4. https://www.ncbi.nlm.nih.gov/pubmed/31484293
5. https://www.sciencedaily.com/releases/2008/03/080314130430.htm
6. https://www.ncbi.nlm.nih.gov/pubmed/15668359
7. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6429313/
8. https://www.ncbi.nlm.nih.gov/pubmed/17081400
9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6017940/
10. https://www.ncbi.nlm.nih.gov/pubmed/15877880
11. https://journals.sagepub.com/doi/pdf/10.1177/1753944709338084
12. https://academic.oup.com/ajh/article/27/7/885/158919
13. https://jakartaglobe.id/lifestyle/watch-your-blood-pressure-to-avoid-kidney-problems/
14. https://academic.oup.com/ajh/article/20/1/21/131236
15. https://www.sciencedaily.com/releases/1999/05/990521055221.htm
16. https://www.sciencedaily.com/releases/2019/07/190711200612.htm
17. https://www.ncbi.nlm.nih.gov/pubmed/11358929
18. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0224975
19. https://www.sciencedaily.com/releases/2012/05/120521163621.htm
20. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5356990/
21. https://www.bloomberg.com/news/articles/2020-03-18/99-of-those-who-died-from-virus-had-other-illness-italy-says
22. https://academic.oup.com/ajh/article/33/5/373/5816609
23. http://pamw.pl/en/issue/article/32231171
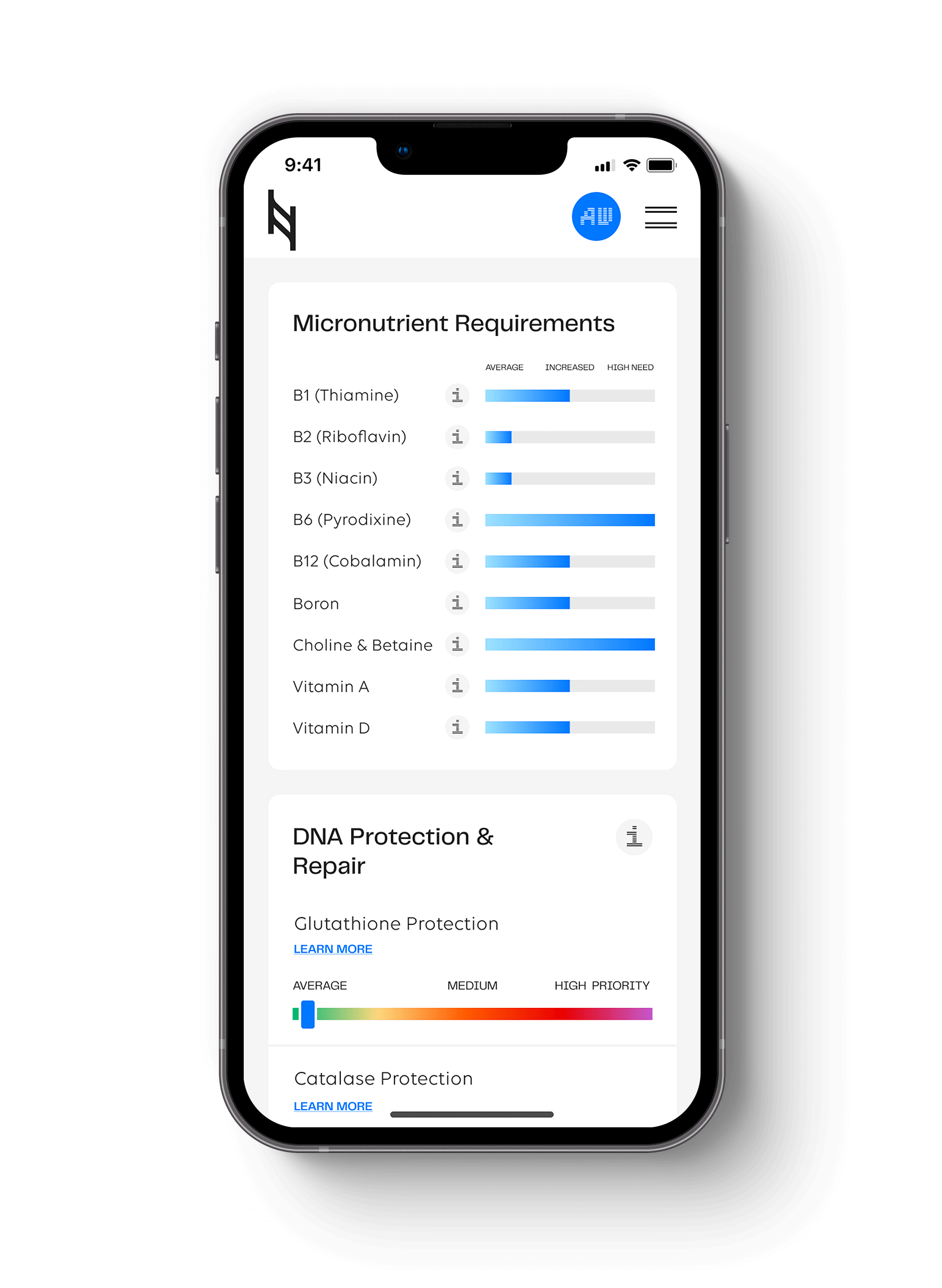
Hit your health goals faster
We'll help you remove the guesswork
Experience the most advanced nutrigenomic test available, covering 100 clinically relevant genes for a "whole body" analysis. Take control of your health today.
$359